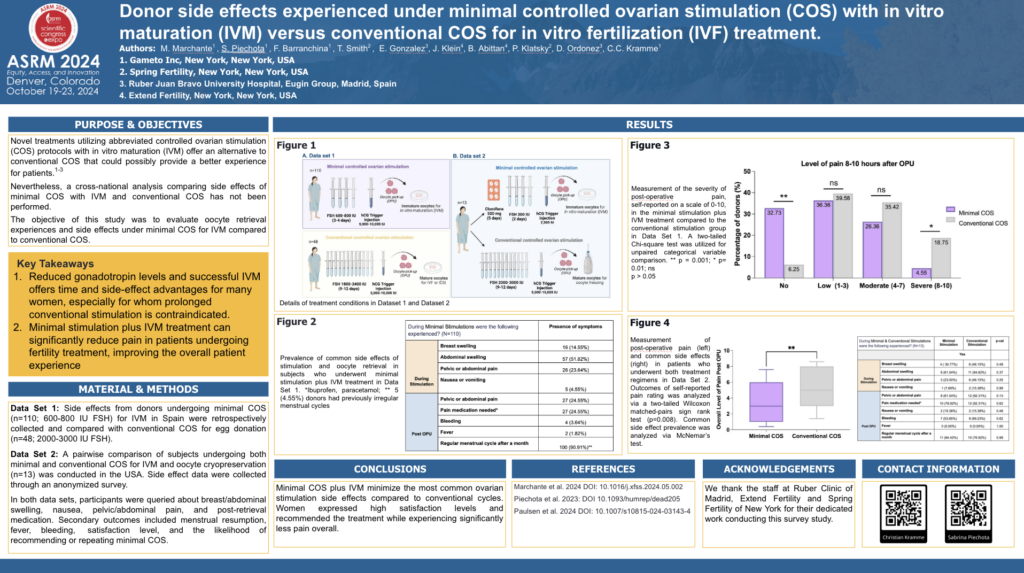
OBJECTIVE: Novel treatments utilizing abbreviated controlled ovarian stimulation (COS) protocols with in vitro maturation (IVM) offer an alternative to conventional COS that could possibly provide a better experience for patients. Nevertheless, a cross-national analysis comparing side effects of minimal COS with IVM and conventional COS has not been performed. The objective of this study was to evaluate oocyte retrieval experiences and side effects under minimal COS for IVM compared to conventional COS.
METHODS AND MATERIALS: This study involved two experimental sets. Side effects from donors undergoing minimal COS (n=110; 600-800 IU FSH) for IVM in Spain were retrospectively collected and compared with conventional COS for egg donation (n=48; 2000-3000 IU FSH).At the same time, a pairwise comparison of subjects undergoing both minimal and conventional COS for IVM and oocyte cryopreservation (n=13) was conducted in the USA. Side effect data were collected through an anonymized survey. Participants were queried about breast/abdominal swelling, nausea, pelvic/abdominal pain, and post-retrieval medication. Secondary outcomes included menstrual resumption, fever, bleeding, satisfaction level, and the likelihood of recommending or repeating minimal COS.
RESULTS: During minimal COS for IVM (data set 1), donors experienced minimal side effects: no breast swelling (86%), no pelvic or abdominal pain (76%), no nausea or vomiting (96%), and no bleeding (96%). After oocyte pick-up, the majority (75%) reported no pelvic or abdominal pain. Compared to conventional COS cycles, minimal COS donors reported significantly less post-retrieval pain, with 33% experiencing no pain (vs. 6%; p=0.0011) and with a reduced severe level of pain (5% vs. 19%; p=0.0097). Overall pain distribution was reduced (p<0.0001), leading to fewer donors requiring pain medication (25% vs. 54%; p=0.0003). Additionally, 85% of women were very satisfied with minimal COSand would recommend or repeat the treatment (86%).
In the comparison in which each subject underwent both treatments (data set 2), women indicated more side effects with the conventional COS, showing increased pain, swelling, nausea or vomiting, medication use, and bleeding compared to minimal COS (p=NS). A reduction in severe pain was observed in minimal COS (8%) versus conventional (38%, p=0.1336), presenting also an overall reduced level of pain (p=0.0078).
CONCLUSION: Minimal COS for IVM minimize the most common ovarian stimulation side effects compared to conventional cycles. Women expressed high satisfaction levels and recommended the treatment.
IMPACT STATEMENT: Reduced gonadotropin levels and successful IVM offers time and side-effect advantages for many women, especially for whom prolonged conventional stimulation is contraindicated.